Resource Library
Find information and resources about stigma and diabetes
Filter
Topic
Type of Resource
I'm
Topic
Type of Resource
I'm
-

Let’s Talk: Diabetes Distress and Burnout
Read More -
How to Talk About Diabetes-Related Complications
Read More -
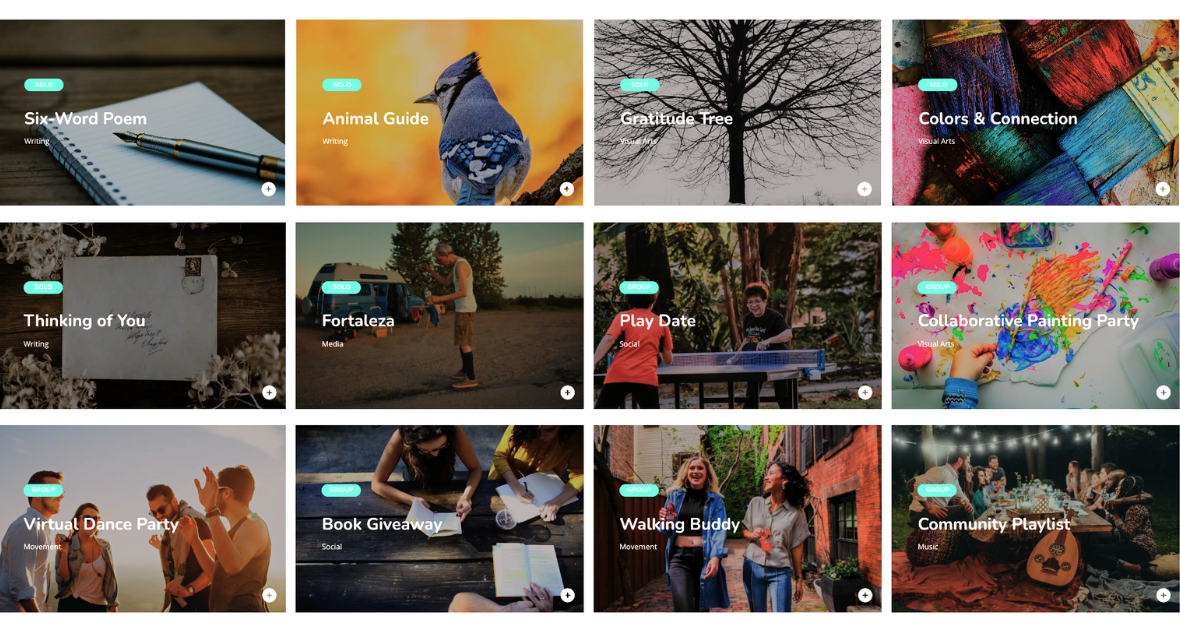
The CreativityHub: Getting UnLonely with Creative Connection
Read More -

Let’s Talk: Diabetes Stigma in Marketing and Communications
Read More -

Let’s Talk: Mental Health & Diabetes
Read More -

Changing the Narrative Around Diabetes
Read More -
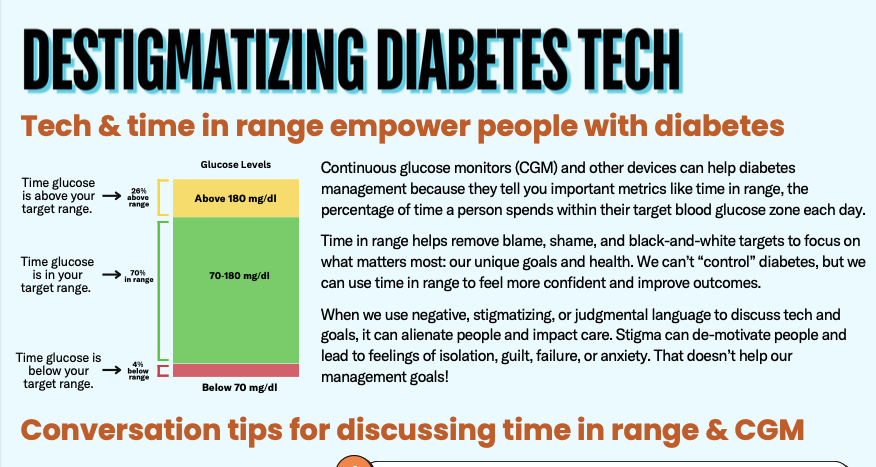
Destigmatizing Diabetes Technology: A Quick Guide
Read More -
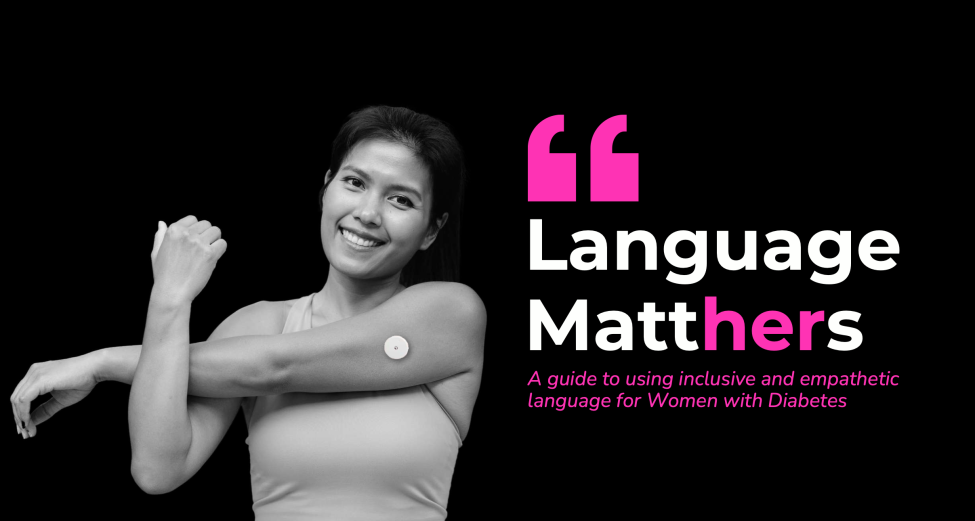
Inclusive Language for Women with Diabetes
Read More -

Connect with Inclusive Diabetes Care Professionals
Read More -

How to Talk About Nutrition with People With Diabetes
Read More -

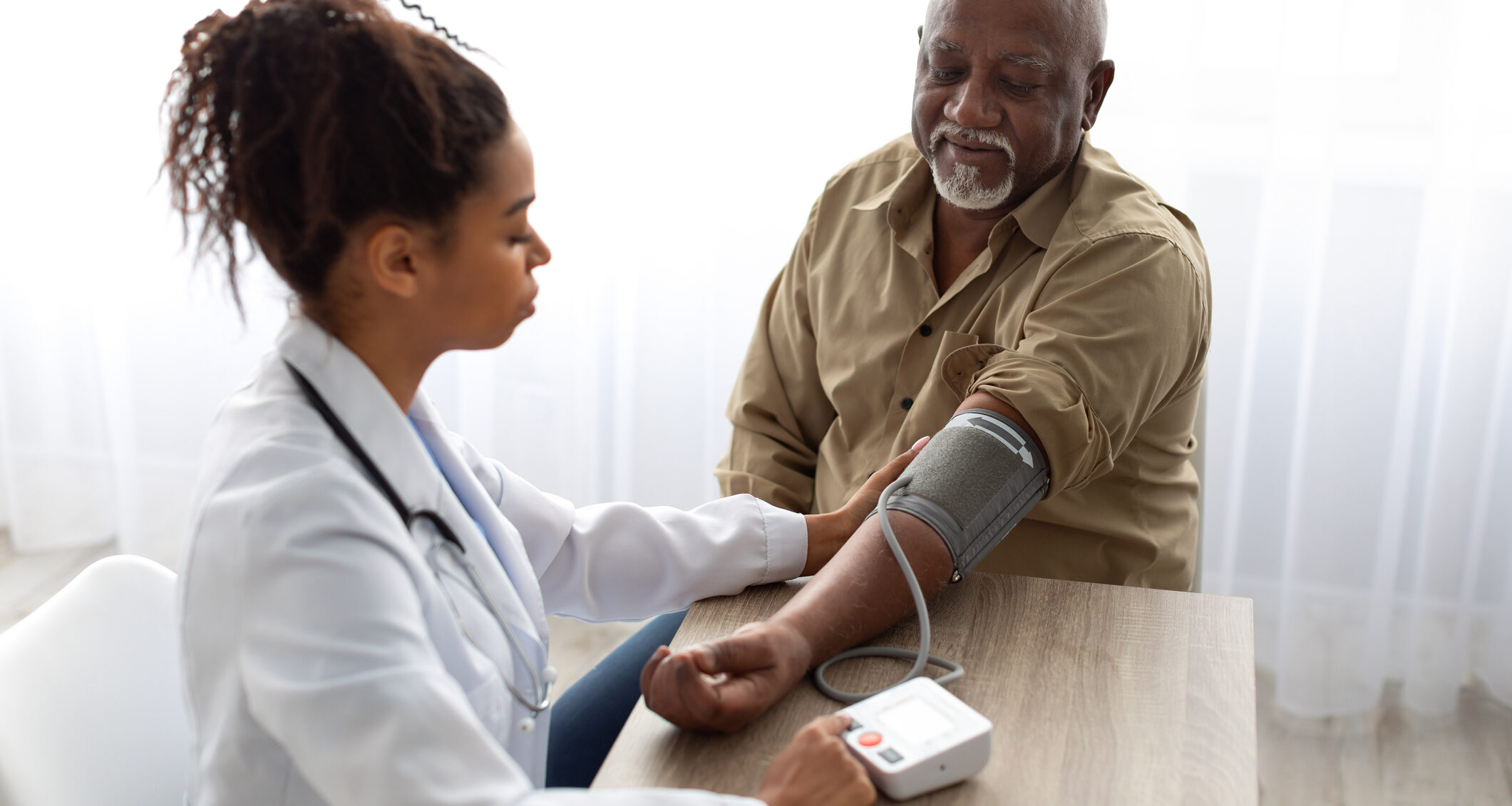
Stigmatizing and Fearful Experiences in the Healthcare Setting
Read More -

dStigmatize Language Guide
Read More