Checking Our Bias: Removing Stigma in the Clinical Setting
Definitions & Background
Diabetes stigma includes the negative stereotypes, blame, judgment, and prejudice that people with diabetes (PWD) experience.1 This type of stigma can lead to discrimination; the unfair or prejudicial treatment of PWD.1
Research suggests as much as 80% of adults with diabetes report experiencing diabetes stigma2 coming from numerous sources: Healthcare professionals (HCPs), the general public, family, friends, colleagues, teachers, peers with diabetes, and the media.1
Diabetes stigma is associated with negative health impacts and behaviors including:
- Depression & anxiety symptoms, diabetes distress, lower self-esteem, & disordered eating.3,4,5,6
- Concealing a diabetes diagnosis & its management.3,4,5
- Reduced diabetes self-management.3,4,5
- Higher HbA1c values & increased severe hypoglycemia risk.7
- Lower quality healthcare interactions, skipped healthcare appointments, & a reluctance to initiate insulin.3,4,5
However, there are limited recommendations on successfully reducing stigma in the clinical setting among HCPs and certified diabetes care and education specialists (CDCES).
Diabetes Stigma in the Clinical Setting
PWD point to the healthcare system and HCPs as a specific source of stigma, reporting that they:
- Feel judged by their HCPs for their HbA1c, Time in Range, lifestyle choices, & weight.4,8,9
- Feel as though their HCPs make assumptions about their diabetes management, weight, & lifestyle choices.4,8,9
- Experience shaming & fear-based messaging as a way to encourage better habits.4,8,9
Experiencing stigma in the healthcare space can drive PWD to:
- Change HCPs (which can be complicated by disparities in access, insurance coverage, & HCP/specialist shortages).4,8,9
- Avoid consultations with HCPs entirely and/or disengage with diabetes self-management.3,4,8
- Seek advice from other sources that may not be able to deliver the same level of care or expertise (family, friends, social media, the internet, etc.).4,8
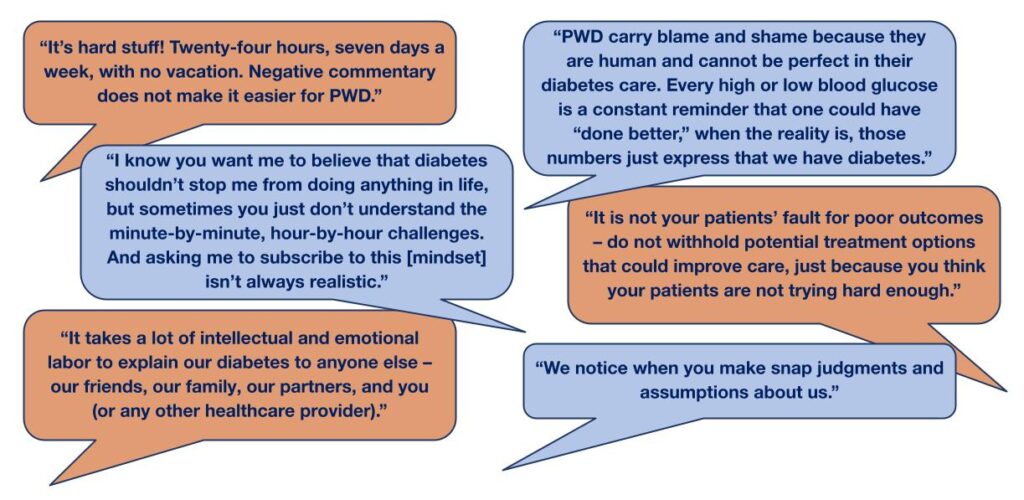
What do People With Diabetes Want You to Know?
In May 2023, diaTribe conducted a small focus group of US adults, including people with type 1 diabetes (n=3), type 2 diabetes (n=1), and caregivers of PWD (parents or HCPs) (n=4). The resulting quotes are taken from the discussion that resulted when presented with the questions: What do you wish healthcare professionals knew about living with diabetes?
The Importance of Language
The language we use to talk about diabetes often reflects a lack of awareness or consideration, and may express conscious or unconscious bias.11,12 Research shows that this language can have lasting negative effects.11,12 Make intentional choices to:
- Use language that is neutral, non-judgmental, and based on facts, actions, or physiology/biology instead of relying on words and phrases that carry a value judgment (good, bad, poor, fail, etc.).11,12
- Use language that is collaborative, supportive, and reflects that PWD are individuals with preferences, priorities, and lives beyond their chronic condition.11,12
- Take a person-centered approach to appointments that is respectful, inclusive, and uses motivational interviewing to show an attention to care and detail, free from assumptions.11,12
- Avoid facial expressions and body language that can contribute to stigma or judgment.

Creating a Stigma- and Judgment-Free Practice
Though interventions aimed at addressing diabetes stigma in the healthcare setting are limited, there are steps you can take to reduce stigma and create a supportive environment for PWD that go beyond language choices.
1. Be mindful of intent vs. impact
- The goal is not perfection. The most important thing is to be mindful that PWD do experience stigma and adjust your practices to minimize this to the best of your ability.
- However, some things that are said or done with good intentions can still negatively impact PWD. Aim to avoid this whenever possible and listen to the diabetes community for best practices.
2. Set up a stigma-free office space
- The physical healthcare space that PWD find themselves in can often contribute to stigma and feel unwelcoming. Aim to set up a clinical space where PWD feel safe and supported, not a place they avoid out of fear.
- Some tips include:
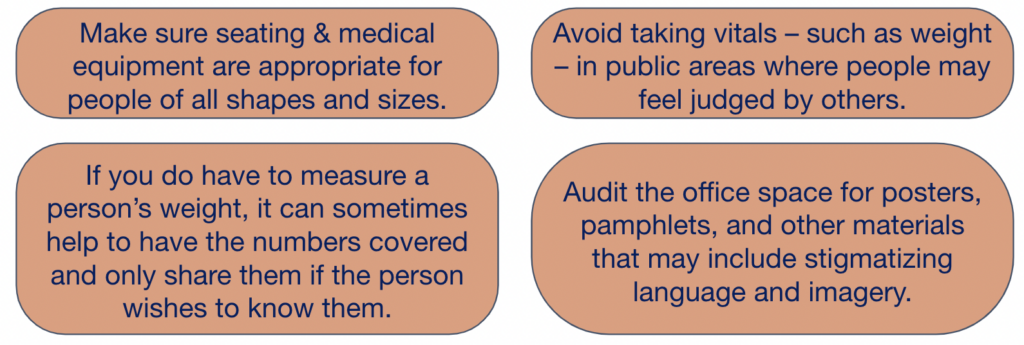
To learn more check out our checklist for Creating a Stigma-Free Clinic.
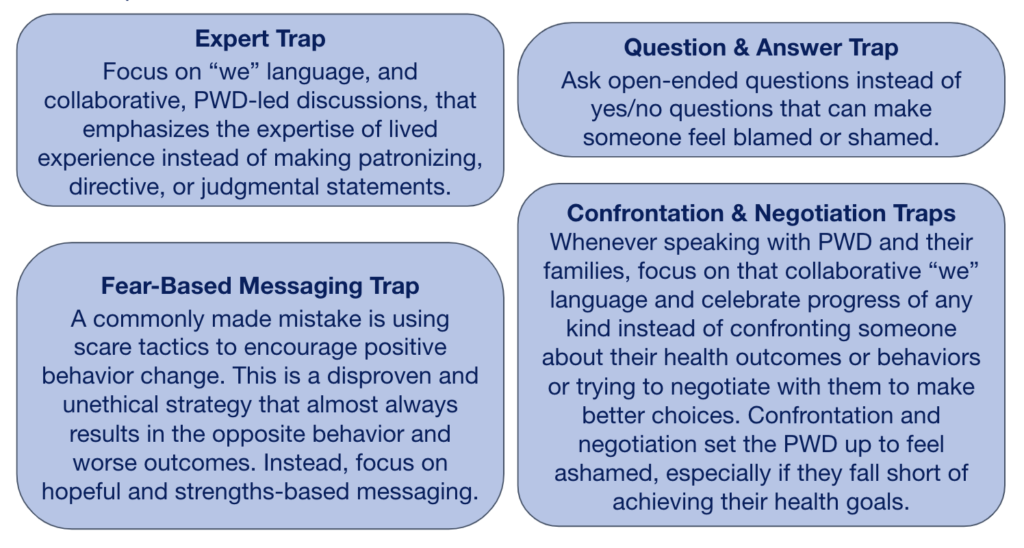
3. Frame conversations and avoid stigmatizing traps
- How we frame conversations and messaging is important. Framing refers to the choices we make – what we emphasize, what we say, and what we don’t say.13
- Effective framing includes avoiding assumptions, blame, or judgment while emphasizing collaboration, empathy, & person-centered messaging.13 Let PWD guide conversations – what are their priorities, their health goals, the challenges they face in their day-to-day lives that prevent them from reaching their goals?
- Some traps to avoid include:
This resource was created for dStigmatize, a diaTribe Foundation program, with support from Lilly Diabetes, AstraZeneca, and the Boehringer Ingelheim-Lilly Alliance.


Citations
- Schabert, J., Browne, J. L., Mosely, K., & Speight, J. (2013). Social stigma in diabetes: a framework to understand a growing problem for an increasing epidemic. The Patient-Patient-Centered Outcomes Research, 6, 1-10.
- Speight J, Holmes-Truscott E, Scibilia R, Black T (2021). Diabetes: Stigma, blame and shame. Diabetes Australia, Canberra.
- Elizabeth Holmes-Truscott, Adriana D. Ventura, Sharmala Thuraisingam, Frans Pouwer, Jane Speight; Psychosocial Moderators of the Impact of Diabetes Stigma: Results From the Second Diabetes MILES – Australia (MILES-2) Study. Diabetes Care 1 November 2020; 43 (11): 2651–2659.
- Browne, J. L., Ventura, A., Mosely, K., & Speight, J. (2013). ‘I call it the blame and shame disease’: a qualitative study about perceptions of social stigma surrounding type 2 diabetes. BMJ open, 3(11), e003384.
- Puhl, R. M., Himmelstein, M. S., Hateley-Browne, J. L., & Speight, J. (2020). Weight stigma and diabetes stigma in U.S. adults with type 2 diabetes: Associations with diabetes self-care behaviors and perceptions of health care. Diabetes research and clinical practice, 168, 108387.
- Puhl, R. M., Himmelstein, M. S., & Speight, J. (2022). Weight Stigma and Diabetes Stigma: Implications for Weight-Related Health Behaviors in Adults With Type 2 Diabetes. Clinical diabetes : a publication of the American Diabetes Association, 40(1), 51–61.
- Hamano, S., Onishi, Y., Yoshida, Y., Takao, T., Tahara, T., Kikuchi, T., … & Kasuga, M. (2023). Association of self‐stigma with glycated hemoglobin: A single‐center, cross‐sectional study of adults with type 1 diabetes in Japan. Journal of Diabetes Investigation, 14(3), 479-485.
- Browne, J. L., Ventura, A., Mosely, K., & Speight, J. (2014). ‘I’m not a druggie, I’m just a diabetic’: a qualitative study of stigma from the perspective of adults with type 1 diabetes. BMJ open, 4(7), e005625.
- Beverly, E. A., Ritholz, M. D., Brooks, K. M., Hultgren, B. A., Lee, Y., Abrahamson, M. J., & Weinger, K. (2012). A qualitative study of perceived responsibility and self-blame in type 2 diabetes: reflections of physicians and patients. Journal of general internal medicine, 27(9), 1180–1187.
- Beverly, E. A., Guseman, E. H., Jensen, L. L., & Fredricks, T. R. (2019). Reducing the Stigma of Diabetes in Medical Education: A Contact-Based Educational Approach. Clinical diabetes : a publication of the American Diabetes Association, 37(2), 108–115.
- Dickinson, J. K., Guzman, S. J., Maryniuk, M. D., O’Brian, C. A., Kadohiro, J. K., Jackson, R. A., D’Hondt, N., Montgomery, B., Close, K. L., & Funnell, M. M. (2017). The Use of Language in Diabetes Care and Education. Diabetes care, 40(12), 1790–1799.
- J, S., T C, S., T, D., T, B., G, K., C, L., R, S., & G, J. (2021). Our language matters: Improving communication with and about people with diabetes. A position statement by Diabetes Australia. Diabetes research and clinical practice, 173, 108655.13. FrameWorks Institute. (2020). Changing the Narrative around Diabetes: A FrameWorks Framing Brief. Washington, DC: FrameWorks Institute.