A Guide to the Portrayal of Diabetes in Film and Television
An accurate and empowering portrayal of diabetes on screen is one of the greatest tools available to raise awareness among the general public and to clear up potentially damaging misconceptions.
This guide was created as a collaboration between the diaTribe Foundation and Beyond Type 1.
Thank you for sharing the realities of living with diabetes with your audience.
Your work will help educate, raise awareness, clear up misconceptions, increase safety, and reduce stigma. Approximately 1.6 million Americans currently have type 1 diabetes ( which includes around 200,000 youth and 1.4 million adults), 34.2 million have type 2 diabetes, and approximately 96 million have prediabetes, a precursor to a possible type 2 diabetes diagnosis. Those numbers are only increasing. Despite how prevalent diabetes is, all types of diabetes are among the most misunderstood and misrepresented conditions out there.

Inaccurate portrayals in film and television fuel common misconceptions about diabetes such as:
- Eating too much sugar or being overweight causes type 1 diabetes.
- Lifestyle choices alone cause type 2 diabetes.
- Type 2 diabetes can always be “reversed” if people try harder.
- All people with diabetes are lazy and unmotivated.
- Only children can develop type 1 diabetes.
- Only adults can develop type 2 diabetes.
- Having diabetes prevents one from participating in high impact sports and physical activities.
- Those with diabetes cannot have any sweets or sugar.
None of these are true.
It is our hope that this guide will provide clarification as to the realities of living with type 1 and type 2 diabetes and will empower media content creators to accurately represent diabetes on screen.
Why Does Accurate Portrayal Matter?
An accurate and empowering portrayal of diabetes on screen is one of the greatest tools available to raise awareness among the general public and to clear up potentially damaging misconceptions.
Mental Health and Stigma
People living with diabetes already carry an immense burden. When they hear inaccurate jokes about how they “did it to themselves” by eating too much sugar or being lazy, or are made the punchline of jokes, it can be psychologically damaging and lead to serious conditions like diabetes burnout, diabulimia, depression, anxiety, etc. Conversely, seeing the accurate representation of people who use diabetes medications and devices (such as insulin, an insulin pump, or a continuous glucose monitor) can help combat the feelings of isolation, loneliness, and anxiety that accompany being a member of an identifiable minority population
Safety
With the best intentions, people make assumptions on how to help people living with diabetes based on what they “learned” from film and television. Unfortunately, this can be dangerous for someone with diabetes, especially those with type 1 – being given an insulin or glucagon shot at the wrong time can be fatal, while being given a source of sugar when it’s not needed can lead to poor health outcomes. Additionally, the idea that shaming or blaming someone for their diabetes will encourage them to make healthier lifestyle choices is incorrect and can actually harm their health and wellbeing.
Openness and Empowerment
When diabetes is discussed openly and honestly in the media by people living with the disease, it can combat some of the stigma surrounding the condition that leads people to hide their diabetes. Accurate representation empowers people to talk openly about their condition with their healthcare teams, family members, and peers – creating a support network that can work together to achieve optimal health for everyone.
What is Type 1 Diabetes?
Type 1 diabetes is a chronic, auto-immune condition that occurs when the body’s own immune system attacks the insulin-producing beta cells of the pancreas.
This attack leaves the pancreas with little or no ability to produce insulin, the hormone that helps regulate blood sugar (also called blood glucose). When this happens, glucose stays in the blood instead of being converted into fuel for the body, causing serious damage to organ systems while depriving the body of fuel.

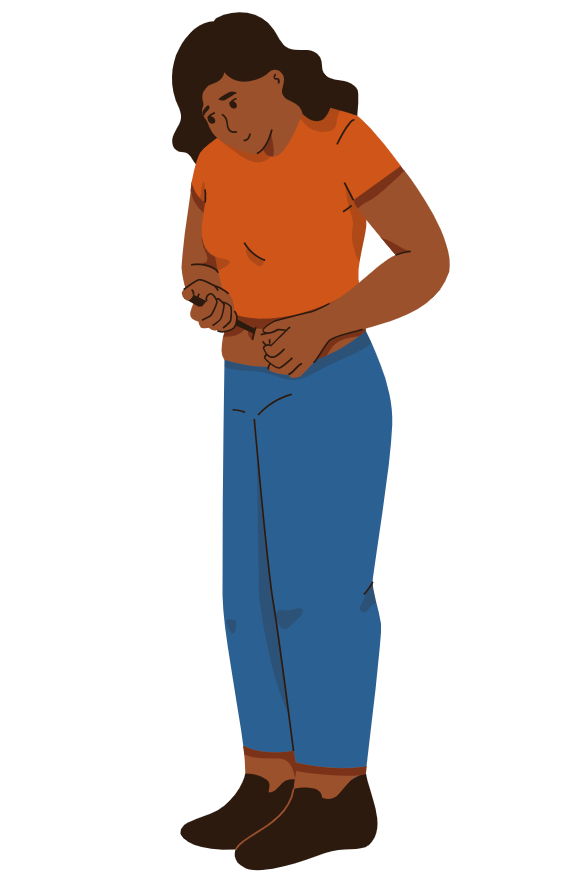
People with type 1 diabetes must inject or pump insulin into their bodies every day to carefully regulate blood sugar and stay alive.
People with type 1 diabetes must take insulin for their entire life. You can be diagnosed at any age – 64,000 people are diagnosed each year in the US; about half are children, half are adults. Even with proper treatment and management of their glucose levels, devastating complications can occur. The condition requires meticulous planning to avoid life-threatening situations.
Currently, it is not possible to prevent, delay, or cure type 1 diabetes. While the exact cause of type 1 diabetes is still unknown, studies suggest that it most likely results from a genetic predisposition, typically combined with an environmental trigger.
What is Type 2 Diabetes?

Type 2 diabetes is a chronic condition that occurs when the body has trouble processing glucose from the blood to use for fuel. This is caused by something called insulin resistance in which the body’s cells do not process insulin correctly.
When this happens, it is characterized by high blood sugar levels, causing serious damage to organ systems while depriving the body of fuel.
People with type 2 diabetes have a variety of treatment options including lifestyle interventions and medications to help them manage their glucose levels and many (though not all) do not require having to take insulin to survive.
People with type 2 diabetes can be diagnosed at any age. Even with proper treatment and management of their glucose levels, devastating complications can occur. The condition requires meticulous planning to avoid life-threatening situations – though it often requires less intensive management than type 1 diabetes.
Currently, it is possible for some people to prevent or delay type 2 diabetes with intensive lifestyle changes. It is also possible for some people to put their type 2 diabetes into remission even after a diagnosis with intensive lifestyle changes. While the exact cause of type 2 diabetes is still unknown, studies suggest that it most likely results from a combination of lifestyle choices and a genetic predisposition, sometimes combined with an environmental trigger.
Representation Examples
Children with diabetes deserve to see themselves on screen – CGMs, insulin pumps, and all
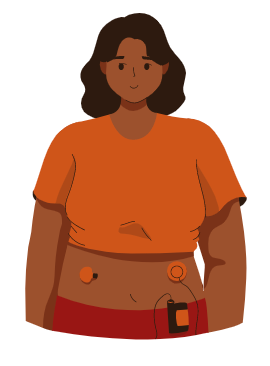
Episode: The Baby-Sitters Club, Season 1 and 2. In The Baby-Sitters Club, one of the main characters, Stacey McGill has type 1 diabetes. On screen, Stacey wears a continuous glucose monitor (CGM) and insulin pump while making decisions that affect her glucose levels. Throughout the show, Stacey becomes more open about her diabetes, leaning on her family and friends for support. She also regularly discusses her glucose levels with her doctor.
What they got right: The show does a lot to accurately portray life with diabetes, from referencing real diabetes organizations like JDRF to showing Stacey interacting with her diabetes devices. The script also makes sure to acknowledge concerns about judgment and shame that people with diabetes often have. Even though Stacey is depicted as a well-liked, social, and stylish teenager, she still has insecurities about her diabetes and what others will think. The show accurately portrays how challenging it can be to manage your diabetes everyday.
When it comes to diabetes, it’s important to make sure myths aren’t reinforced
Episode: Black-ish, Season 4, Episode 9, “Sugar Daddy.” During this episode, the main character, Dre, is diagnosed with type 2 diabetes. He is in denial at first and after a chaotic meeting at work in which many misconceptions about diabetes are discussed as fact, he becomes fearful. When Dre’s father shows him a documentary claiming diabetes can be “cured,” Dre begins fasting and ends up passing out at a party, having not eaten or taken his medications. The episode ends with his wife, Bow, supporting him as he tries checking his blood sugar for the first time and realizing it doesn’t hurt. She explains that diabetes is completely manageable and she is there to help in any way she can.
What they got right: The show does a good job portraying the realities of a diabetes diagnosis. The main character, Dre goes through a wide range of emotions throughout the episode, including some fear and hesitation around checking his blood sugar and giving himself medicine. However, the show makes it a point to highlight that diabetes is a manageable condition, and his wife (who plays a doctor) in the show supports him throughout the process. The show also does a good job highlighting the many misconceptions that people have about diabetes – including the idea that fringe diets and supplements can cure a person’s diabetes.
What missed the mark: The episode introduces a lot of myths about diabetes – that all people with diabetes lose decades off their lives, that they are going to “lose their feet,” and that you can cure diabetes with an assortment of fringe diets and supplements, among many others. However, the show doesn’t go quite far enough in making sure these myths are disproved. Though the episode implies that many of these misconceptions are false, they never explicitly correct these statements.
Even kids can be the “food police,” if they don’t really understand how diabetes works
Episode: Hannah Montana, Season 2, Episode 30, “No Sugar, Sugar.” During the episode, it is revealed that one of the main characters, Oliver, has diabetes. His friends, who don’t quite understand what this means, spend the rest of the episode trying to keep him away from anything sweet that has sugar. When they finally have a conversation about it, Oliver explains that he actually can eat sweets, so long as he manages his blood sugar and takes his medicine, and that he was scared to tell them because he didn’t want them to view him as “broken.” His friends say that they wish he had told them so they could understand more and support him – and they apologized for being the “food police.”
What they got right: The episode does a lot right. The episode accurately portrays common misconceptions about diabetes. It also described the ways they can be harmful to people with diabetes, especially when friends and family think it’s their job to police what people can and can’t do. In addition, Oliver explains that diabetes doesn’t inherently mean you don’t want to, or can’t, have sweets, and it explores the internalized stigma and shame that many people with diabetes feel.
What missed the mark: The show oversimplifies the differences between type 1 and type 2 diabetes, insinuating that people with type 2 diabetes should avoid sweets while people with type 1 can eat them. In addition, it oversimplifies and inaccurately depicts the process of checking a person’s blood sugar and encourages the idea that all you have to do to correct a low blood sugar is to eat sweets.
Diabetes can be funny, but it should never be the punchline of a joke

Episode: Big Bang Theory, Season 8, Episode 1, “The Locomotion Interruption.” Toward the end of the episode, one of the main characters is interviewing for a sales job at a pharmaceutical company. When describing how her previous job experience as a waitress has prepared her for this job, she explains that she, “Convinced a lot of very large customers who should not be eating cheesecake to have more cheesecake.” She goes on to say that, “One of those chubsters even had an insulin pump.”
What missed the mark: Unfortunately, this episode chose to make diabetes the punchline of a joke about people with obesity. Using the word “chubsters” and mentioning the fact that one of the patrons had an insulin pump inaccurately and offensively insinuates that all people with excess weight have diabetes, and that they shouldn’t be allowed to have a dessert.
Appendix: Glossary of Terms
A1C – Your A1C measures the quantity of sugar attached to your red blood cells. A1C provides an estimate of your average blood sugar level over the past two to three months; higher blood sugar levels are associated with higher A1C levels. An A1C of 6.5% or higher indicates the presence of diabetes.
Automated Insulin Delivery – The development of automated insulin delivery has many names – artificial pancreas, hybrid closed loop, bionic pancreas – but all share the same goal: using continuous glucose monitors and smart algorithms to automatically adjust insulin delivery via pump to keep a person’s glucose levels in range.
Blood Glucose Meter – Blood glucose meters measure a person’s blood sugar level at the specific moment of checking. To use a meter, people insert a test strip into the meter, prick their finger with a lancing device to draw blood, and then put a small drop of their blood onto the test strip. The meter gives a blood glucose reading in mg/dl (US standard) or mmol/l (European standard).
Continuous Glucose Monitor – Continuous glucose monitors (CGM) measure the body’s glucose levels in real-time by sensing the glucose present in tissue fluid (also called interstitial fluid). While a blood glucose meter provides a measurement of the blood glucose level at a specific moment in time (when you prick your finger), CGMs typically provide a new glucose level every five minutes, meaning 288 times per day.
Diabetic Ketoacidosis – Ketoacidosis, or diabetic ketoacidosis (DKA) in people with diabetes, occurs when a person does not have enough insulin to provide glucose to cells for energy. The body responds by breaking down its fat stores (into ketones) for energy, resulting in high levels of ketones in the blood. Ketones are acidic molecules, so an increased level of ketones can cause the blood to become more acidic – which prevents the body from functioning fully. DKA can be life threatening and must be treated immediately.
Gestational Diabetes – Gestational diabetes can develop during pregnancy, if a woman’s body cannot produce enough insulin to keep blood sugar levels in a target range. Gestational diabetes is usually temporary, and blood sugar levels will often stabilize after childbirth.
Glucagon – Glucagon is a hormone (a natural chemical made by your body) that prompts the body to release stored sugar into your bloodstream. Glucagon is used to treat people with diabetes for severe hypoglycemia at home.
Glucose levels, blood sugar levels – Blood sugar, or blood glucose, comes from the food that we eat and serves as our body’s main source of energy. Your blood sugar level refers to the amount of glucose in your blood at a specific moment in time.
Hyperglycemia – Hyperglycemia (high blood sugar) is defined as a glucose value above 180 mg/dL. Hyperglycemia is often a result of insufficient insulin, not enough physical activity, or too much food (particularly those high in carbohydrates). Over time, hyperglycemia can lead to major long-term health complications.
Insulin – Insulin is a critical hormone in the body that facilitates the uptake of glucose into the cells and lowers blood sugar levels. People with type 1 diabetes and some people with type 2 diabetes need to take insulin because their bodies either cannot produce enough insulin (insulin deficiency) or cannot respond well to their own insulin (called insulin resistance).
Insulin Pump – Insulin pumps are devices that deliver insulin in the body without the need for manual injections. They are able to administer rapid-acting insulin in both basal (slow) and bolus (mealtime) capacities, and often come with built-in bolus dose calculators.
Hypoglycemia – Hypoglycemia (low blood sugar) is defined as a glucose value below 70 mg/dL. Hypoglycemia is usually a result of diabetes treatment, often because there is too much insulin in the body. Common symptoms of hypoglycemia include hunger, sweating, and fatigue. Severe hypoglycemia can result in seizures and loss of consciousness.
Latent Autoimmune Diabetes in Adults (LADA) – LADA is a slow-progressing form of autoimmune diabetes. Like type 1 diabetes, in LADA, your pancreas stops producing enough insulin. But unlike type 1, with LADA, you often won’t need insulin for several months up to years after you’ve been diagnosed and the condition is often diagnosed in people over the age of 30. This often means that people who have LADA are misdiagnosed with type 2 diabetes initially.
Other diabetes drugs – For people with type 2 diabetes, there are other common drugs that help lower blood glucose levels. Each one has a slightly different mode of action, and they can have varying effects and benefits depending on the person. These include: metformin, SGLT-2 inhibitors, GLP-1 receptor agonists, sulfonylureas (SFU), thiazolidines (TZD), and DPP-4 inhibitors.
Prediabetes – Prediabetes is a reversible condition in which the body has higher than normal blood sugars. If left unnoticed or untreated, blood sugars can continue to rise, resulting in type 2 diabetes.
Time in Range – Time in Range (TIR) is the percentage of time that a person spends with their blood glucose levels in a target range. The range will vary depending on the person, but general guidelines suggest a range of 70-180 mg/dl for most people with diabetes. TIR can be measured using a CGM.